Kraft Prediabetes Profile: Patterns Overview
A Summary of Dr. Kraft’s Data:
Dr. Kraft, a clinical pathologist, ran 3,650 glucose-insulin tolerance tests. Dr. Kraft was looking for diabetes mellitus and was not particularly looking for hypoglycemia. Many of his tests were ran for only three hours or four hours. For this reason, the new Kraft Prediabetes Profile should not only yield more information as outlined below with regard to the diagnosis of diabetes mellitus and latent glucose tolerance tests, but it also should enable us to do more for hypoglycemia. Of the 3,650 glucose tolerance tests, 1,713 were defined a normal (for diabetes mellitus) according to the criteria of the American Diabetes Association.
Of the 1,713 tests which would have been judged normal strictly on the basis of glucose tolerance, 50% were demonstrated abnormal on the basis of insulin tolerance, and another 14% were borderline results. 2.5% were displayed insulin response.
This means that 2/3 of the tests that would have been judged normal by the Glucose Tolerant Test were found to be latent diabetic when the Kraft Prediabetes Profile test was taken into consideration.
Remember that all these people were referred because of suspicion of diabetes, so the high numbers should not be so surprising, but what the above data shows is that of the 1,713 cases, out of 3,650 which would have been judged normal by only glucose tolerance test criteria, the insulin test showed that only one third of them really were normal.
Looking at the overall group of 3,650 people referred because of suspicion of diabetes, the usual glucose tolerance test criteria would have found that 1713 were normal. Bringing to bear the insulin tolerance test, two thirds of these so-called “normal” tests were found to be latent diabetic. It appears obvious that the glucose-insulin tolerance test will detect many more latent diabetics.
Criteria for the Kraft Prediabetes Profile are as follows. This is once again as taken from the article by Dr. Kraft:
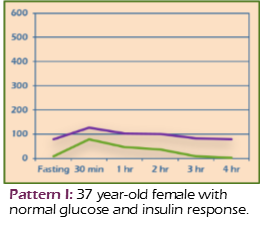
Pattern I: Normal
- Normal fasting insulin 0-10 units
- Peak insulin at ½-1 hour
- 2nd hour insulin <50
- 3rd hour insulin < 2nd hour
- 2nd hour + 3rd hour totals < 60
- Subsequent values at fasting range (0-10)
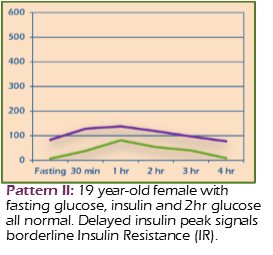
Pattern II: Delayed Insulin Peak
- Normal fasting insulin 0-10 units
- Peak insulin at ½-1 hour
- 2nd hour + 3rd hour totals > 60 and <100 = Borderline insulin resistance
- 2nd hour + 3rd hour totals > 100 = definite insulin resistance
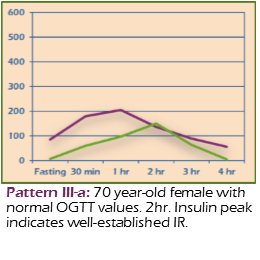
Pattern III A: Insulin Resistance
- Normal fasting insulin 0-10 units
- Peak insulin at 2nd hour
- Considered diagnostic for insulin resistance
- Glucose tolerance may be within normal limits or impaired
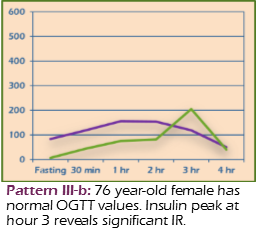
Pattern III B: Insulin Resistance
- Normal fasting insulin 0-10 units
- Peak insulin at 3rd hour
- Considered diagnostic for insulin resistance
- Glucose tolerance usually at diabetic levels
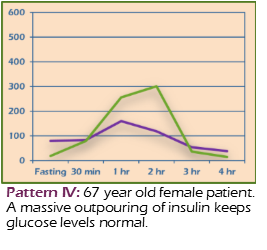
Pattern IV: Insulin Resistance
- Fasting insulin >10
- Diagnostic for insulin resistance
- Glucose tolerance usually at diabetic levels
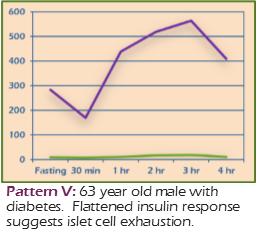
Pattern 5: Insulinopenic
- When glucose levels are elevated, this is considered to be a Type I DM pattern
- All tested values for insulin <30
- Insulin insufficiency probably due to damaged or exhausted islet cells
- Glucose tolerance usually at diabetic levels
- May signal the need for exogenous insulin
- When seen with normal glucose values, may be indicative of a low carbohydrate diet
Dr. Kraft’s article discusses only latent diabetes. In another article by Dr. William Hudspeth, associate professor of psychiatry form the University of Nevada School of Medicine, it is pointed out that frequently hypoglycemic symptoms do not correlate with the low point on a glucose tolerance test. It is pointed out that they also may have occurred despite a fairly normal looking glucose tolerance test. Dr. Hudspeth’s group has evaluated this phenomenon further by running insulin tolerance along with glucose tolerance and at the same time putting an EEG on each patient and observing for brain wave response.
Unfortunately, we’re not going to be able to do an EEG and pick up the abnormal brain wave response. What’s interesting is that Dr. Hudspeth found in some cases the glucose was low and in other cases it was normal. What seemed to correlate better with hypoglycemic symptomatology was either low or normal glucose in combination with a distinct insulin peak.
Although Dr. Hudspeth did not have a breakdown of the different types of patterns, just this information alone should enable us to better pick up hypoglycemic symptomatology in the absence of abnormal glucose tolerance test values.
References:
Detection of Diabetes Mellitus, In Situ (occult diabetes), Kraft, Joseph R., Laboratory Medicine, Volume VI, #2, pages 10-22, February 1975.
Neurobiology of the Hypoglycemia Syndrome, Hudspeth, W.J. Et Al, Journal of holistic Medicine, Volume III, #1, pages 60-71, Spring/Summer, 1981.
