What makes a gut “leaky” and what can be done about it?
In addition to food digestion, the gastrointestinal tract is one of the body’s primary defenses against the external environment. The loss of these intestinal defenses is commonly called “leaky gut”, and it may contribute to food allergy and food sensitivity reactions.1 Increased intestinal permeability (“leakiness”) can contribute to chronic inflammatory disease and increase the risk of food allergy or food sensitivity reactions. In most cases, normal permeability can be restored once the causative factors are identified and corrected.
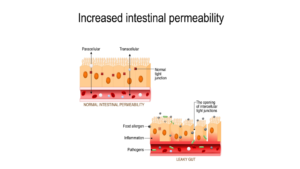
The lining of the gastrointestinal system (the intestinal mucosa) is constantly coming into contact with the foods we eat and swallowed inhalants, such as plant pollens or dust.2 Proteins found in foods or inhalants are antigens, toxic or foreign molecules that provoke an immune response in the body. Since the gut mucosa is exposed to antigens from the external environment every day, a large proportion of the immune system’s lymphoid immune tissues are associated with the gastrointestinal system. Normally, the physical lining of the gut, in combination with the intestinal lymphoid tissues, the secreted mucus layer and the commensal intestinal bacteria (the gut microbiome) form a protective barrier. The barrier is semi-permeable, and allows nutrients to pass through the gut lining into circulation.3 The intestinal barrier blocks antigens and pathogenic (disease-causing) microbes from entering the body. In a healthy digestive system, the immune system response to antigen exposure is non-reactive tolerance. In a dysregulated system, some antigens provoke the immune system, resulting in an allergic response or food sensitivity.
If the intestinal barrier is compromised, the permeability increases. As permeability increases, larger and more antigenic molecules can slip through the intestinal barrier into the bloodstream. Once the antigens have crossed the barrier or entered the circulation, they may trigger local or systemic inflammatory responses. Local inflammatory responses will cause symptoms in the gastrointestinal tract. Systemic responses may occur anywhere in the body and be responsible for stiff joints, nasal congestion, and other symptoms.
The permeability of the intestinal barrier may be compromised by a variety of factors, including digestive function, genetics, diet, nutritional status, toxic exposures, lifestyle and composition of the gut microbiome.4,5 These factors may affect the function of the gastrointestinal tract, the immune system, or the gut microbiome, and ultimately increase the risk of food allergy or sensitivity:
Digestive function
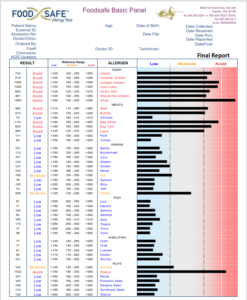
The proper digestion of proteins, fats and carbohydrates creates smaller antigen molecules that the immune system can more easily handle. Any medical condition that prevents complete protein digestion may increase the risk of food allergy and food sensitivity.4 Insufficient levels of digestive enzymes or gastric hydrochloric acid prevent proper digestion and nutrient absorption. Poor gut motility (diarrhea or constipation) also prevent proper digestion. Food allergies or sensitivities may increase the inflammation of the gastrointestinal lining, increasing permeability and “leakiness”. A stool analysis and food sensitivity testing may be a good first step in assessing the digestive process.
Genetics
Abnormal digestion and absorption of nutrients may be acquired or inherited.6 An acquired condition is often reversible, but an inherited condition may require life-long management. Inherited conditions may include Celiac disease, lactose intolerance, digestive enzyme deficiency (particularly carbohydrate enzymes), altered gut barrier, poor immune system function, or impaired transportation of nutrients into the body. Inflammation may influence genetic expression and contribute to chronic disease, allergic responses and food sensitivities.5 Inflammation may result from poor diet, malnutrition, toxic exposures, psychological stress or disruption of the gut microbiome. Avoidance of problem foods, proper nutrition, combined with healthy diet and lifestyle, may counteract or minimize the effects of inflammation and inherited differences.7
Diet and nutrition
Studies in animals and humans indicate that low-fiber, processed diets high in trans-fats and simple carbohydrates are pro-inflammatory. Such diets disrupt the gut microbiome, increase intestinal permeability and gut “leakiness”.3,8 Inflammation of the gut lining may promote systemic inflammation, inhibit production of carbohydrate-digestive enzymes, prevent the absorption of nutrients, and result in dysbiosis (imbalance) of the gut microbiome. Both under- and over-nutrition may be harmful: a lack of necessary nutrients and amino acids can inhibit immune functions or promote pro-inflammatory signaling, while excess calories promote obesity and inflammation. The ingestion of xenobiotics (substances unnatural to the system) in the diet can exacerbate the inflammatory response to a poor diet. Diets high in complex carbohydrates (fiber) and fresh or frozen plant foods help to decrease inflammation and restore balance to the microbiome.
Toxic exposures
Xenobiotics include chemicals and toxic metals that can dysregulate the immune system, promote inflammation and disrupt both digestion and the gut microbiome. Xenobiotics include artificial colors and sweeteners found in packaged foods or genetically-modified foods containing pesticides. Other exposures may be inhaled and then swallowed. These inhalant exposures may include food or other proteins found in house dust, chemicals from household items or food packaging, toxic metals in food or water, and air pollution particulates.9,10 These xenobiotics may affect the human host, promoting inflammation or inhibiting key enzyme functions in metabolic, detoxification and immune systems. Xenobiotic exposures may affect the gut microbiome, altering microbe populations into a dysbiotic profile that promotes local and systemic inflammatory signaling.
Lifestyle
The level of cortisol produced during an experimental stressor has been directly correlated with the level of intestinal permeability in human subjects, and the inflammatory mechanism, mast cell activation, is common to both the stress and antigen-response (allergy/sensitivity) pathways.11 Stressors whether physical, such as extreme exercise, or psychological have an enormous impact on digestive functions, the immune system and the gut microbiome.12 Stressors shut down the parasympathetic “rest and digest” system and activate the sympathetic “fight, flight or freeze” system which increases inflammation and inhibits normal digestion. Stress-related signaling hormones from the brain induce changes in the intestinal barrier that alter the gut microbiome and increase intestinal permeability and “leakiness”. Stressors in the womb or in early childhood may prime the gut for leakiness throughout life into adulthood, and may contribute to disorders such as food allergy or sensitivity. Stressors may also cause functional gastrointestinal disorders such as indigestion or irritable bowel, and inflammatory bowel diseases.13

Gut microbiome
The bacteria and other microbes that live in our gastrointestinal tract form a community called a “microbiome”.14 In a healthy microbiome, different groups of bacteria, such as lactobacillus and bifidobacteria, breakdown the indigestible starches left behind after the digestion process and create metabolic products that can be exchanged among various members of the microbiome. Some of the synthesized bacterial products are nutritive vitamins are absorbed by the human host and contribute to host health.15 Disruptions in the gut microbiome may occur due to the poor digestion, introduction of pathogens, toxic exposures, poor diet, or psychological stress. The use of certain medications, such as stomach acid suppressors (“H2-blockers”), can also alter the microbiome.5 A diet rich in fiber, fruits and vegetables increases the diversity of the gut microbiome and the levels of beneficial bacteria, which is a sign of gastrointestinal health.12
Restoration of the gut barrier
Fortunately, there are different ways to improve digestion and restore intestinal barrier functions.16 Consult with a health-care provider to obtain any necessary testing and treatment protocols.
- Relax
- A variety of mind-body methods may promote the “rest and digest” signaling needed to normalize digestion, inflammation, immune functions and the gut microbiome.17 Researched techniques include mindfulness, cognitive behavioral therapy, meditation, and yoga. Early evidence indicates that relaxation practices affect not only the parasympathetic nervous system, but decrease DNA expression of inflammatory protiens.
- Reduce
- Identify and eliminate toxic exposures wherever possible.18 Test drinking water for toxic metals, and use water filters when necessary. Reduce the consumption of GMO products, artificial colors and sweeteners, and highly processed foods. Processed foods may contain small amounts of trigger foods that can perpetuate allergic responses and food sensitivity.19 Buy foods frozen or in glass containers whenever possible to minimize plastics exposures, and transfer foods out of microwaveable containers or packaging prior to heating to reduce chemical exposures.
- Alcohol use can increase intestinal permeability and gut “leakiness”; therefore, reduce or eliminate consumption.20
- Medications may affect digestion or cause gastrointestinal inflammation.5 Consult with a healthcare provider and pharmacist prior to discontinuing any prescribed medications.
- Remove
- Remove pathogens, dysbiotic bacteria, or fungal overgrowths identified during stool testing.21
- Foods that cause any sort of digestive symptoms may contribute to poor digestion or local intestinal inflammation. Remove known allergens and food sensitivities.8,22 Less reactive or “moderate” response foods may be eaten on a rotation plan.
- Replace
- Replace hydrochloric acid and digestive enzymes as indicated by symptoms (gas, bloating, heartburn) gastric analysis and stool testing.
- Replace trans-fats and simple carbohydrates with healthy omega-3 fatty acids and fiber-rich foods.
- Reinoculate
- Probiotics are a good first step, but do not permanently colonize the gastrointestinal tract in all individuals.23 Probiotics work best when a healthy diet full of fiber, fruits and vegetables is also consumed.
- Incorporate a variety of fermented foods into the diet to promote colonization by Lactobacillus and other species.24
- Repair
- Gastrointestinal and systemic inflammation can be reduced, and normal immune functions restored, by using a food allergy/sensitivity free diet and stress reduction. The addition of supportive nutrients such as butyrate, curcumin, glutamine, selenium, zinc, vitamins A and D also promote the healing of the intestinal barrier.25 A diet rich in fiber, fruits and vegetables will provide both fiber and antioxidant and anti-inflammatory plant compounds.
Increased intestinal permeability can contribute to chronic inflammatory disease and increase the risk of food allergy and food sensitivity reactions. In most cases, “leakiness” can be reduced and permeability can be restored once the causative factors are identified and corrected.
References:
1. Vighi G, Marcucci F, Sensi L, Di Cara G, Frati F. Allergy and the gastrointestinal system. Clin Exp Immunol. 2008;153 Suppl 1(Suppl 1):3–6.
2. Faria AM, Gomes-Santos AC, Gonçalves JL, et al. Food components and the immune system: from tonic agents to allergens. Front Immunol. 2013;4:102.
3. Samadi N Klems M Untersmayr E. The role of gastrointestinal permeability in food allergy. Annals of Allergy, Asthma & Immunology. 2018;121(2):168-173.
4. Pali-Schöll I, Untersmayr E, Klems M, Jensen-Jarolim E. The Effect of Digestion and Digestibility on Allergenicity of Food. Nutrients. 2018;10(9):1129.
5. Gigante G, Tortora A, Ianiro G, Ojetti V, Purchiaroni F, Campanale M, Cesario V, Scarpellini E, Gasbarrini A. Role of gut microbiota in food tolerance and allergies. Dig Dis. 2011;29(6):540-9.
6. Vancamelbeke M, Vanuytsel T, Farré R, et al. Genetic and Transcriptomic Bases of Intestinal Epithelial Barrier Dysfunction in Inflammatory Bowel Disease. Inflamm Bowel Dis. 2017;23(10):1718–1729.
7. Abdul QA, Yu BP, Chung HY, Jung HA, Choi JS. Epigenetic modifications of gene expression by lifestyle and environment. Arch Pharm Res. 2017 Nov;40(11):1219-1237.
8. Myles IA. Fast food fever: reviewing the impacts of the Western diet on immunity. Nutr J. 2014;13:61.
9. Sheehan WJ, Taylor SL, Phipatanakul W, Brough HA. Environmental Food Exposure: What Is the Risk of Clinical Reactivity From Cross-Contact and What Is the Risk of Sensitization. J Allergy Clin Immunol Pract. 2018 Nov – Dec;6(6):1825-1832.
10. Rosenfeld CS. Gut Dysbiosis in Animals Due to Environmental Chemical Exposures. Front Cell Infect Microbiol. 2017;7:396.
11. Vanuytsel T, et al. Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Gut. 2014 Aug;63(8):1293-9.
12. Kelly JR, Kennedy PJ, Cryan JF, Dinan TG, Clarke G, Hyland NP. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392.
13. Wu JC. Psychological Co-morbidity in Functional Gastrointestinal Disorders: Epidemiology, Mechanisms and Management. J Neurogastroenterol Motil. 2012;18(1):13–18.
14. Shreiner A, Kao J, Young V. The gut microbiome in health and in disease. Curr Opin Gastorenterol. 2015 Jan;31(1):69-75.
15. Rowland I, Gibson G, Heinken A, Scott K, Swann J, Thiele I, Tuohy K. Gut microbiota functions: metabolism of nutrients and other food components. Eur J Nutr. 2018 Feb;57(1):1-24.
16. Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2011 Dec;62(6):591-9.
17. Buric I, Farias M, Jong J, Mee C, Brazil IA. What Is the Molecular Signature of Mind-Body Interventions? A Systematic Review of Gene Expression Changes Induced by Meditation and Related Practices. Front Immunol. 2017 Jun 16;8:670.
18. Sears ME, Genuis SJ. Environmental Determinants of Chronic Disease and Medical Approaches: Recognition, Avoidance, Supportive Therapy, and Detoxification. J Environ Public Health. 2012;2012:356798.
19. Sheehan WJ, Taylor SL, Phipatanakul W, Brough HA. Environmental Food Exposure: What Is the Risk of Clinical Reactivity From Cross-Contact and What Is the Risk of Sensitization. J Allergy Clin Immunol Pract. 2018 Nov – Dec;6(6):1825-1832.
20. Vancamelbeke M, Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol. 2017 Sept;11(9):821-834.
